The following article was written by Eagle Staff Writer Eric Jankiewicz and published in the Butler Eagle Special Sections on October 6, 2020.
Taking the Team Approach: Butler VA customizes care for women vets
Benefits available to help patients with breast cancer
The Butler VA Health Care staff knows its female veterans. They are more likely to have experienced sexual abuse than their male counterparts during service and are often diagnosed with post-traumatic stress disorder.
These issues can affect all other aspects of their health — including a fight with breast cancer.
To face that battle, the Butler VA takes a team approach, tailoring the blend of medical professionals to the unique needs of each patient.
The Butler VA, which covers five counties, served 26,964 unique patients in its 2019 fiscal year. Of those veterans served, 1,903 or 7%, were female. Unique patients refers to veterans who have received at least one care service from their health care system in 2019.
At least 1 in 3 woman who receive medical treatment from the Veterans Health Administration have reported sexual trauma during their military service, according to Summer Drummond, the Butler VA Women’s Health Program manager and maternity care coordinator.
And, she said, post-traumatic stress disorder is the most commonly diagnosed issue for female veterans. In the region, female patients often also suffer from obesity, hypertension, and back problems. Another frequent diagnosis is breast cancer. October is breast cancer awareness month, but at the Butler VA prevention of breast cancer is always a priority, according to Drummond.
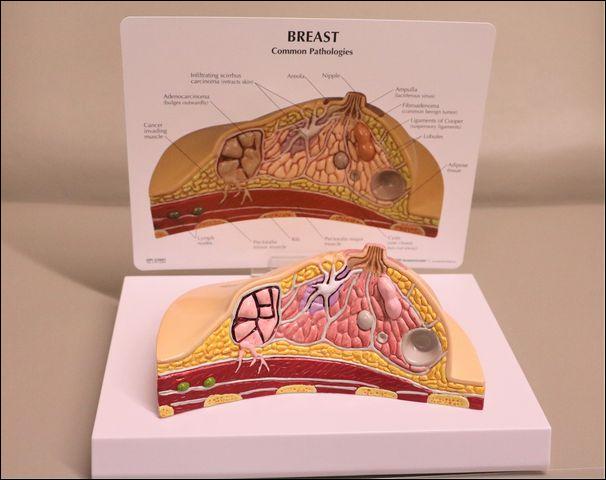
Besides skin cancer, breast cancer is the most commonly diagnosed cancer among American women, according to the Centers for Disease Control and Prevention. But in Pennsylvania the rate is higher at 1 out of 7, according to Drummond.
Help for women with breast cancer
“So it’s very important to screen our vets,” said Drummond, who is also a licensed registered nurse. “The VA has great benefits for women.”
With that in mind, they recommend breast screening annually between the ages of 40 to 54 and then every other year after that.
If a woman being treated at the VA has breast cancer and undergoes a mastectomy — the medical term for the removal of one or both cancerous breasts — the center can provide items to help the veterans feel more comfortable: the list includes mastectomy bras, breast prosthetics, mastectomy bathing suits and other specialized gear.
If a patient undergoes chemotherapy and suffers from hair loss as a side effect of the treatment, the VA will provide wigs to their patients for as long as they are needed.
Typically, new patients at the VA will be assessed for how likely they are to get breast cancer, according to Dr. Erica Hoffman. Hoffman is a women’s health provider, chief of staff at the Butler VA and a member of the executive leadership team. She said that patients receive genetic counseling: the process of determining how likely a patient is to get diseases like breast cancer based on their family history.
Health teams & Whole Woman Care
“Our vets are very engaged in their care,” Hoffman said. “Once people come to the VA, they receive a lot of care here and then we provide Whole Woman Care.”
Hoffman described Whole Woman Care as a holistic approach to a patient’s well-being.
To do that, there are 11 women’s health teams, which are made up of various medical experts that work together to address all the needs of patients assigned to their teams. Each team has a doctor, nurse, medical assistant, dietitian and other experts.
“When you’re going through something scary like breast cancer, it’s nice to have a whole team at your back,” Hoffman said. Drummond added, “When you have cancer, it affects a number of things.”
The assembled health care team tackles any issues that arise. For female patients, all-women teams can be assigned if the patient has suffered sexual abuse from a man. Through all of these considerations, Hoffman said that the VA as a government health-care provider exceeds the private sector in most ways.
“We have more programs that help people stay healthy and improve their health,” Hoffman said, noting that they often do better than the private sector because a lot of their work with patients is focused around prevention.” Hoffman said that in the private sector, only 68% of eligible patients were screened for breast cancer but at the VAs about 83% of those eligible were screened.
“It’s because we’re a one-stop shop. We have it all here,” Hoffman said, adding that the health teams allow a patient’s treatment to not miss a beat between specialists and services. “Imagine you’re a patient having to figure out where to go and who’s covered by your insurance. But here you don’t have to figure out if a specialist is covered,” Hoffman said.
Focus on women’s health
Drummond said the Butler VA will be looking to hire more female-focused specialists to fill a growing demand for women’s care. Along with breast cancer screening and treatment, the Butler VA also offers other services like infertility treatment and reproductive health.
For women and men, the VA can help with infertility treatment or contraception. They also offer in vitro fertilization.
“We then try to closely monitor a patient through the life of pregnancy,” Drummond said. The health care center also helps with end of life care, tracking women for end of life issues like osteoporosis, menopause and urinary conditions. And for those who need it, they have community live in centers and adult day health care.